It could be more than just wheezing and coughing.
Sometimes, you encounter symptoms like the two and think that you have a common cough or allergies, but that may not be the case. It might be asthma and you won’t even know it.
Keeping your respiratory health in check is important especially during this time of the COVID-19 pandemic. It helps your body absorb oxygen to promote regular blood circulation and it keeps your other organs functioning properly. In keeping your respiratory conditions healthy, you can:
- Eat a healthy diet
- Avoid pollutants that may damage your airways
- Exercise regularly
- Consult with your doctor regularly
Asthma is a common respiratory condition that requires immediate and frequent medical attention. Here are some things you need to know about it.
What is Asthma?
 Photo courtesy of cottonbro via Pexels
Photo courtesy of cottonbro via Pexels
Asthma, as defined by Healthline, is a common inflammatory disease where your airways swell and produce extra mucus, causing them to narrow. This causes shortness of breath and can trigger coughing, wheezing, and difficulty breathing.
But what most people don’t know is that asthma has more than one classification. This National Asthma Week, we’ll be breaking the common misconceptions of the disease so you could be provided with accurate information.
The classifications of asthma include:
- Intermittent Asthma
- Mild Persistent Asthma
- Moderate Persistent Asthma
- Severe Persistent Asthma
Intermittent Asthma
A person is considered to have intermittent asthma when their symptoms occur not more than twice a week, and asthma flare-ups don’t usually exceed more than twice a month.
Among the symptoms of intermittent asthma include:
- Difficulty breathing
- Wheezing
- Chest tightness
- Coughing
While these are very common symptoms, it’s important to keep in mind that asthma classifications are differentiated with how many times they occur with the patient, and how it affects their daily activities. In the case of intermittent asthma, this condition doesn’t usually affect one’s daily life, and sometimes does not have symptoms at all.
Treatments for intermittent asthma include a doctor’s prescription for short-acting beta-agonists or inhalers that can help reduce wheezing and difficulty breathing.
Mild Persistent Asthma
Conditions like mild persistent asthma often occur at least twice a week or at least two nights a month. Symptoms of mild persistent asthma include:
- Wheezing or whistling during breathing
- Coughing
- Swelling
- Mucus development in your airways
Unlike intermittent asthma, mild persistent asthma may affect daily activities. For example, it may develop into exercise-induced asthma or the type of asthma triggered by strenuous exercise.
Mild persistent asthma can be developed by people who have a family history of asthma, smoking or second-hand smoking, allergies, and people suffering from weight conditions.
Treatment for mild asthma usually involves quick-acting bronchodilators like rescue inhalers for asthma flare-ups and allergy-relieving medicine for asthma attacks worsened by allergic reactions.
Moderate Persistent Asthma
If a patient has moderate persistent asthma, they tend to have increasingly severe symptoms on a daily basis and at least once a week during the night. Flare-ups are also often occurring and may last longer than usual.
People with this condition experience coughing and wheezing that can affect their daily activities. These symptoms can also cause nighttime flare-ups that can affect your sleep routines. Other symptoms include:
- Chest tightness
- Chest pain
- Shortness of breath
- Swollen, inflamed or mucus lining in the airways
- Coughing
In treating moderate persistent asthma, doctors may prescribe medications and treatments that help reduce the daily symptoms the patient experiences and reduce the occurrence of flare-ups.
Long-term medications include doctor-prescribed inhaled corticosteroids, pills, and combination inhalers. Rescue inhalers and allergy medications can also be prescribed in case of emergency flare-ups.
Severe Persistent Asthma
The last classification of asthma, and probably the most dangerous, is severe persistent asthma. With this condition, patients are likely to experience symptoms of asthma several times a day and even during the night.
Severe persistent asthma can be experienced by anyone. It can start as one of the classifications above and develop severely later on. It is important to look after your health if you have a family history of asthma, smoking, or second-hand smoking, allergies and if you have experienced pneumonia.
Treating severe persistent asthma is a little more difficult and aggressive. As asthma is a chronic condition and therefore does not have any cure, medications would only help manage the symptoms you’re experiencing.
Sometimes, inhaled corticosteroids and oral corticosteroids will be given at higher doses. Rescue inhalers and medications will also be given to prevent triggers from occurring.
How to Prevent Asthma Attacks
 Photo courtesy of Mockup Graphics via Unsplash
Photo courtesy of Mockup Graphics via Unsplash
Asthma is caused by both genetic and environmental factors around you. And while there are no definite steps to prevent your asthma attacks from happening, the best step to take is to avoid encounters with your triggers.
Here are some reminders from our respiratory experts to help reduce asthma attacks from happening:
1. Identify your triggers
 Photo courtesy of Towfiqu Barbuiya via Unsplash
Photo courtesy of Towfiqu Barbuiya via Unsplash
The first step in preventing asthma attacks is to identify your triggers. Asthma triggers are environmental conditions that may cause your attacks. These include:
- Air pollution
- Allergens, or those that trigger your allergies
- Exercise
- Weather condition
- Smoke, and a lot more
In finding out your asthma triggers, it is helpful to keep an allergy diary with you so you’re able to detail all the factors that affect your asthma. Regular consultations with a pulmonologist could also help in figuring out your triggers and how you could prevent attacks from happening.
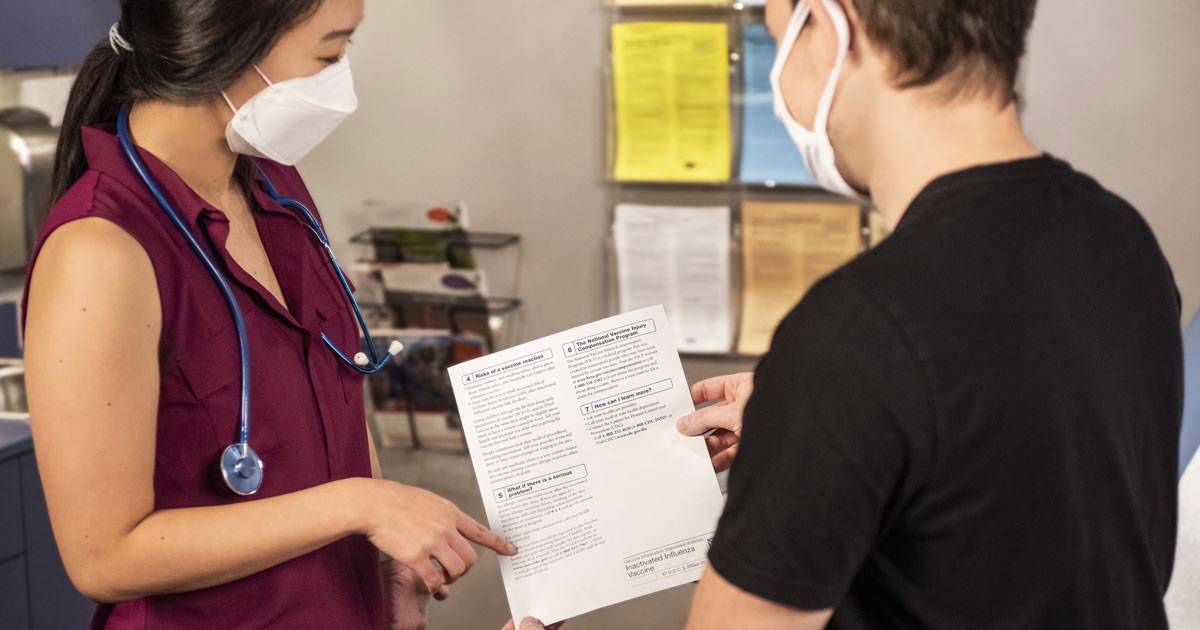
2. Regular vaccinations
 Photo courtesy of CDC via Unsplash
Photo courtesy of CDC via Unsplash
Flu and pneumonia can also be contributing factors to worsening asthma conditions and vice versa. Help prevent worsening conditions by getting your annual flu shot and pneumonia shot once every 5 to 10 years.
You can also get allergy shots or immunotherapy to help prevent allergy symptoms to help keep your allergy at bay. Consult with a doctor to know what is best for you.
3. Take your prescribed asthma medication
 Photo courtesy of Adam Niescioruk via Unsplash
Photo courtesy of Adam Niescioruk via Unsplash
If you have prescribed medicine from your doctor to help manage your asthma, make sure to take them religiously no matter the circumstances. Regular medications will help reduce your asthma attacks by a significant number.
It is also important to keep an eye out on how much you use your rescue inhalers. If you find yourself using our emergency inhalers too often than usual, then it’s time for you to schedule a consultation with your doctor.
4. Consider using an Air Filtration System
 Photo courtesy of Alvaro Bernal via Unsplash
Photo courtesy of Alvaro Bernal via Unsplash
If allergens are one of the reasons for your asthma attacks, then you can clean up the air around you with a high-efficiency air filter.
Having equipment with air filtration systems can help get rid of the pollutants in your home so you could breathe cleaner air. However, not all devices can remove small allergen particles.
It is best to combine the use of air filters with other methods that can help control your asthma triggers and symptoms.
For some, asthmas may be a simple set of symptoms. But if not managed well, it may lead to worsening or even fatal conditions. If you’re experiencing any recurring symptoms of asthma, book an appointment with the pulmonologists at The Hospital at Maayo.





























Leave a Reply